EXTERNAL RADIOTHERAPY
- 4 Elekta accelerators, with multileaf collimators and on-board imaging (“Conebeam CT”),


- 1 Accuray Cyberknife accelerator,
- 1 dosimetric scanner,
- Logiciel of planification : Ray station
BRACHYTHERAPY
Definition
Brachytherapy is an irradiation technique consisting in implanting one or several radioactive sources close to or even within the tumor itself.
The treatment directly targets the area of the cancer. In certain locations (cancer of the prostate, the endometreum, the uterus) the irradiation is systematically chosen in view of attacking te tumor while sparing the healthy surrounding tissues.
Brachytherapy for patients in Poitou-Charentes is organized through multidisciplinary meetings of the regional network in which surgeons, organ specialists and oncologists are associated. As a “recourse” treatment, brachytherapy often supplements the surgery and radiotherapy delivered within the region.
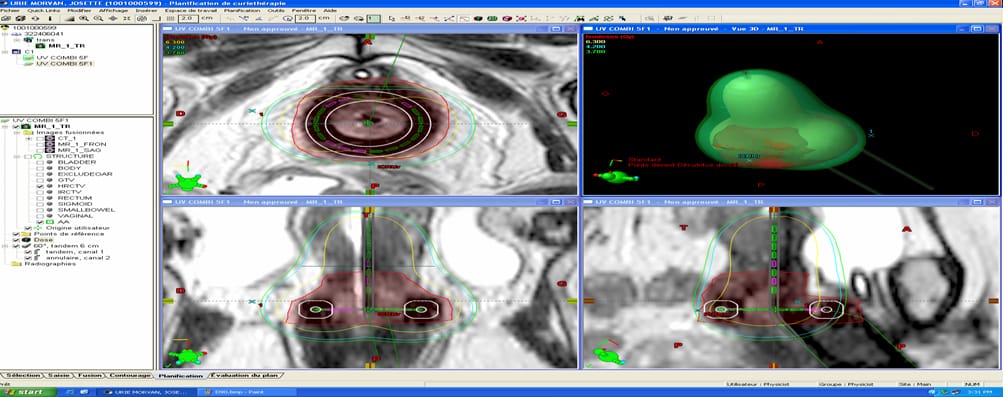
Since 2009 the Poitiers CHU has had a modern high-flow regional brachytherapy unit equipped with a protected application room, a HDR afterloader, access to modern imagery (scanner and MRI, echo-doppler) and dosimetry and 3D navigation software. The Poitiers CHU contains a hospitalization section with 6 beds and carries out 200 brachytherapies a year in weekday hospitalization or outpatient treatment.
Two types of brachytherapy are proposed for patients according to type of tumor and stage of cancer.
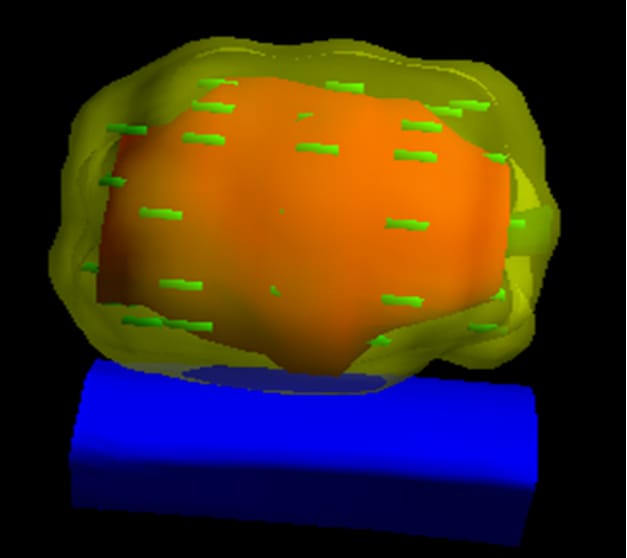
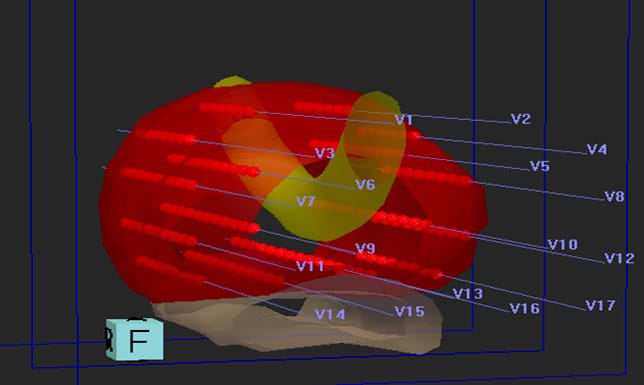
- Iodine 125 brachytherapy is used only for treatment of intraprostate cancers for which clinical evaluation shows no risk of general disease. Through application of this technique,iodine 125 grains are permanently implanted. The CHU team has developed real-time brachytherapy by 3D navigation on ultrasound and magnetic resonance image. This kind of brachytherapy “boosts” the intraprostatic cancer cell concentrations by optimizing the positions of the iodine grains within the prostate. Since 2000, the Poitiers CHU has carried out 850 implants and provided training for 12 European centers. The technique is applied on an inpatient or outpatient basis.
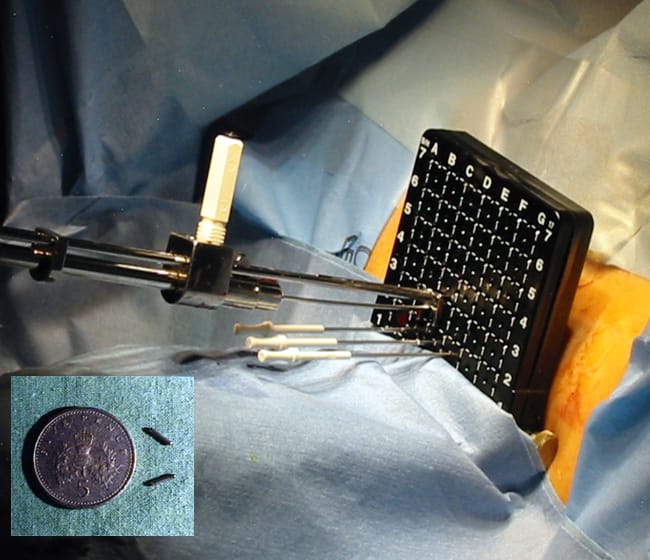
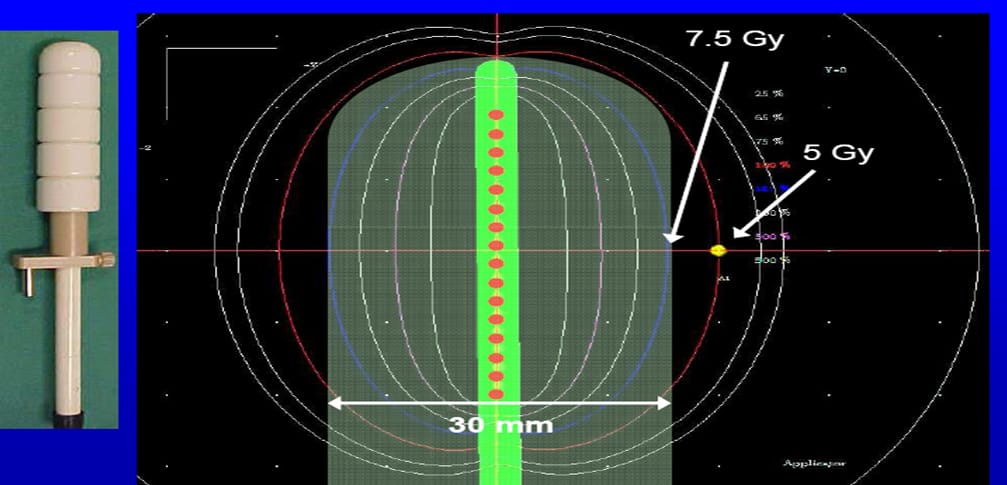
- High dose rate (HDR) brachytherapy uses a small-sized radioactive source (0.3 x 4 mm) that is displaced little by little within the vectors positioned in the tumor to be irradiated. A monitored robot moves and modulates stoppage times in the vectors according to the proximity to the tumor of each vector position. The treatment is brief, lasting only a few minutes and being repeated one to nine times a week. It is carried out either in outpatient or weekday hospitalization. It is delivered either after five sessions of radiotherapy (two nights) or without radiotherapy in nine sessions (four nights). Brachytherapy sessions take place in a protected room in the vicinity of the brachytherapy technical platform. The initial brachytherapy consultation often takes place under anesthetic gas so as to improve patient comfort.

Locations treated by brachytherapy (HDR)
- Endometrial cancers : Outpatient brachytherapy is often carried out to prevent recurrence on the vaginal fundus. It takes place once a week either without radiotherapy in four sessions or after radiotherapy in two sessions.
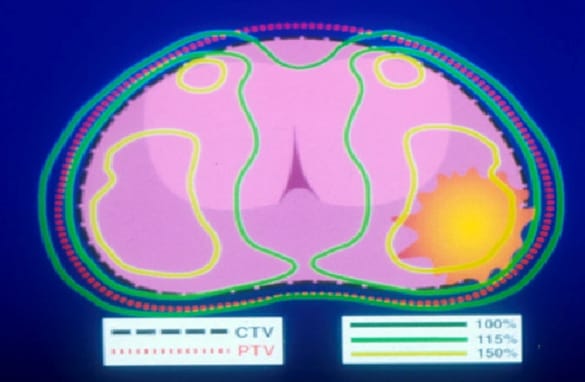
- Cervical cancer : Utero-vaginal brachytherapy involves application of a uterine probe and a non-invasive vaginal ring; during this treatment, the cervix and the fornix (cul-de-sac or dead end) are irradiated. In cases of cancer that are locally advanced (parametrial, vaginal extensions) or unresponsive after radio-chemotherapy, vectors can be associated with the utero-vaginal applicator to treat tumor extensions not covered by the applicator. After positioning of the applicator under general anesthesia or spinal anesthesia, 3D dosimetry is carried out on MRI.
- Prostate cancer : This from of brachytherapy is applied in addition to external local-regional radiotherapy for prostate cancer that is locally advanced and of intermediate prognosis. Brachytherapy boost at once protects healthy tissues (rectum, bladder) and allows for escalating doses on the intraprostatic tumor zones. Application of the technique necessitates two nights of hospitalization. Irradiation is carried out in real time in two sessions, one of them taking place six hours after the other.
 |
 |
- Vaginal cancer : This form of brachytherapy is employed either on a stand-alone basis or as a supplement to external local-regional radiotherapy; hospitalization lasts either two or four nights.
- Anal cancer : This form of brachytherapy is employed as a supplement to external local-regional radiotherapy for localized hemi-circumferential cancers, hospitalization involves five sessions and lasts two nights.
- ENT cancer : The locations susceptible to benefit from brachytherapy are the orificial zones (eyelids, lip, nose, tongue). This form of brachytherapy can be carried out on an outpatient basis or during a hospital stay involving nine sessions and lasting four nights.
- Skin cancer : This form of brachytherapy is often employed after the failure of local outpatient treatments or during a hospital stay involving five sessions and lasting two nights.
- Penis cancer : This form of brachytherapy is carried out in cases of localized penis cancer during a hospital stay involving nine sessions and lasting four nights.
- Keloid formation (excessive granulation) : Brachytherapy is carried out as a supplement to keloid exeresis in order to control scarring; it takes place either on an outpatient basis or during a hospital stay involving five sessions and lasting two nights.
- Breast : One-week HDR brachytherapy is under evaluation in the United States as a possible alternative to conventional external radiotherapy; it is delivered in six weeks for localized forms with a favorable prognosis in postmenopausal women.
- Perioperative HDR brachytherapy : The technique consists in positioning vectors in the tumor area remaining inaccessible to surgery during a surgical operation. The patient is subsequently treated by brachytherapy.
